Wool blankets have been the standard for managing hypothermic combat casualties from the past (WWI) to recent (Operation Iraqi Freedom/Operation Enduring Freedom) conflicts. It wasn’t until 2006 that the CoTCCC published the first hypothermia prevention guidelines to address a high rate of trauma-induced hypothermia in combat casualties, and recommended a non-insulated Hypothermia Prevention and Management Kit (HPMK), containing an outer vapor barrier garment and a 8-hour Ready-Heat Blanket II (38°C/100°F in ten minutes). The HPMK is a lightweight, small dimension, vacuum-sealed kit, and is low cost. The HPMK became one component of the Joint Theater Trauma System’s theater-wide strategy to address hypothermia in battlefield casualties. However, in 2019 Dutta et al. selected human volunteers for exposure in a cold (-22°C/-8°F) chamber, and evaluated the effectiveness of the HPMK and four other active heated hypothermia enclosure systems. The results indicated that the HPMK, as compared to four insulated active heated hypothermia enclosure systems, was ranked the lowest in both subjective ratings and objective physiological heat transfer and balance indices.
These findings by Dutta et al., and along with feedback from military units regarding HPMK limitations in cold weather resulted in the CoTCCC Hypothermia Working Group addressing three specific questions in their review and made conclusions regarding enclosure rewarming systems for management of all-cause hypothermia – see Table 2.
Table 2: Enclosure Warming System Questions, Conclusions, and Strength of Evidence.
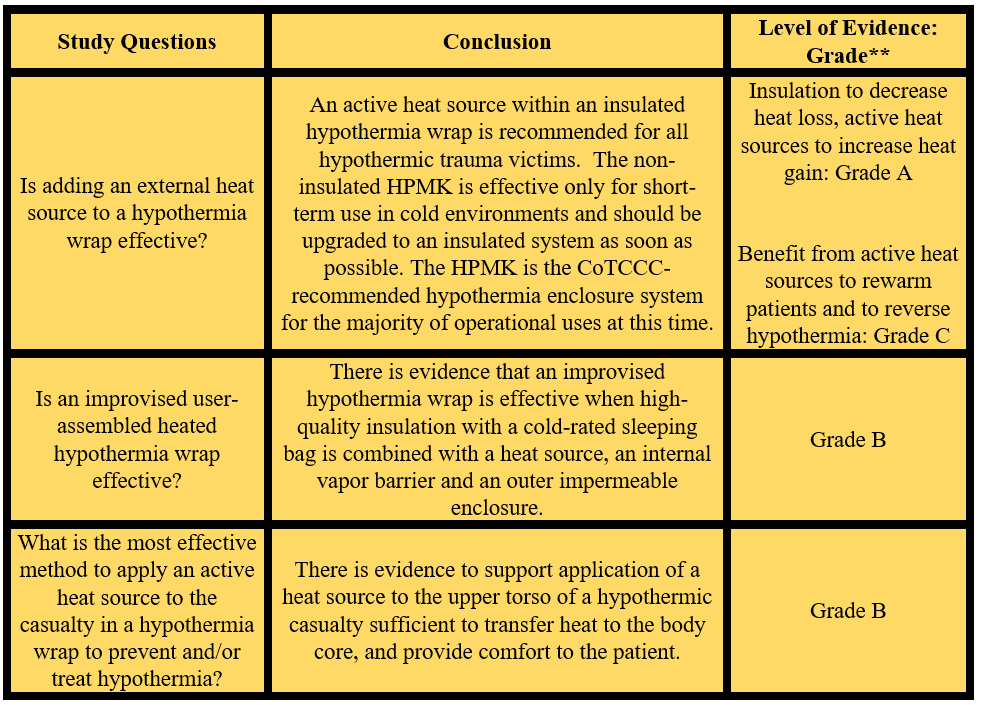
**The levels of evidence used by the American College of Cardiology and the American Heart Association were outlined by Tricoci P, et al. 2009.
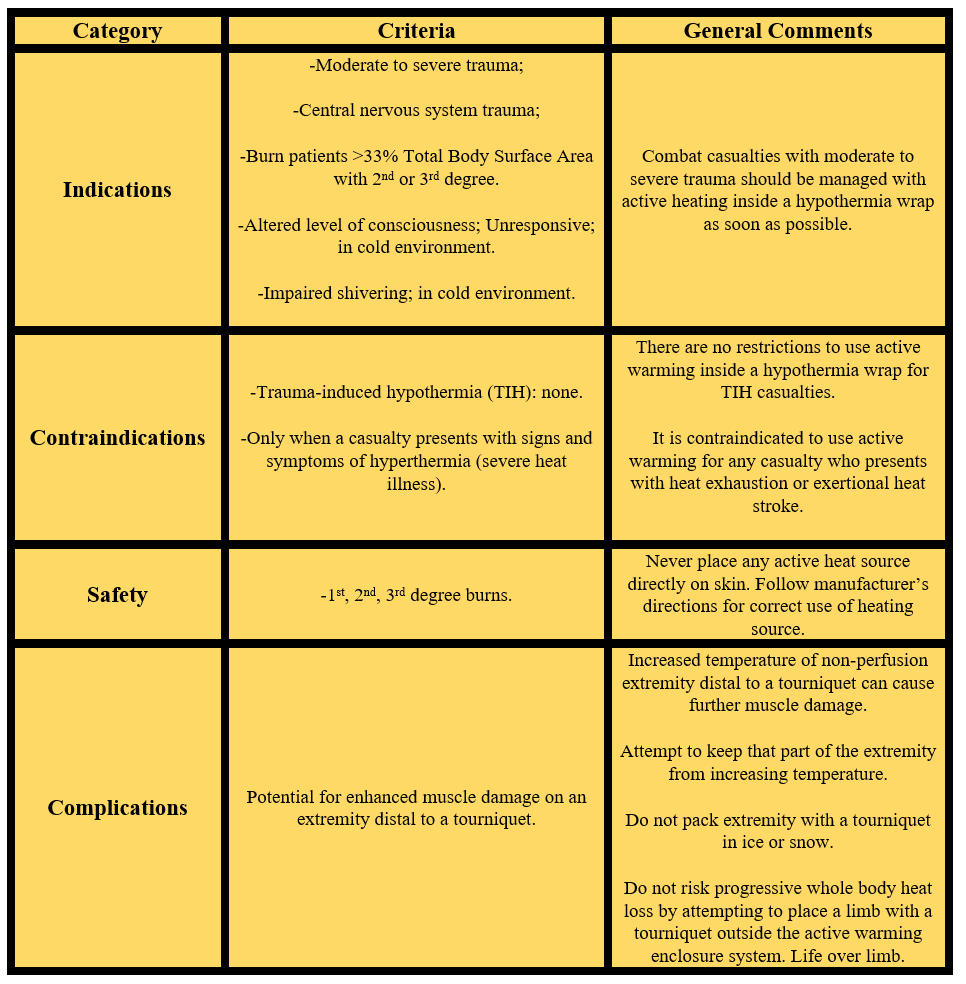
Also addressed by the CoTCCC Hypothermia Working Group was the following: What are the indications, contraindications, safety, and complications when adding an external heat source inside a hypothermia wrap during field management? This is summarized in Table 3.
Table 3. Indications, Contraindications, Safety, and Complications for Active Rewarming.
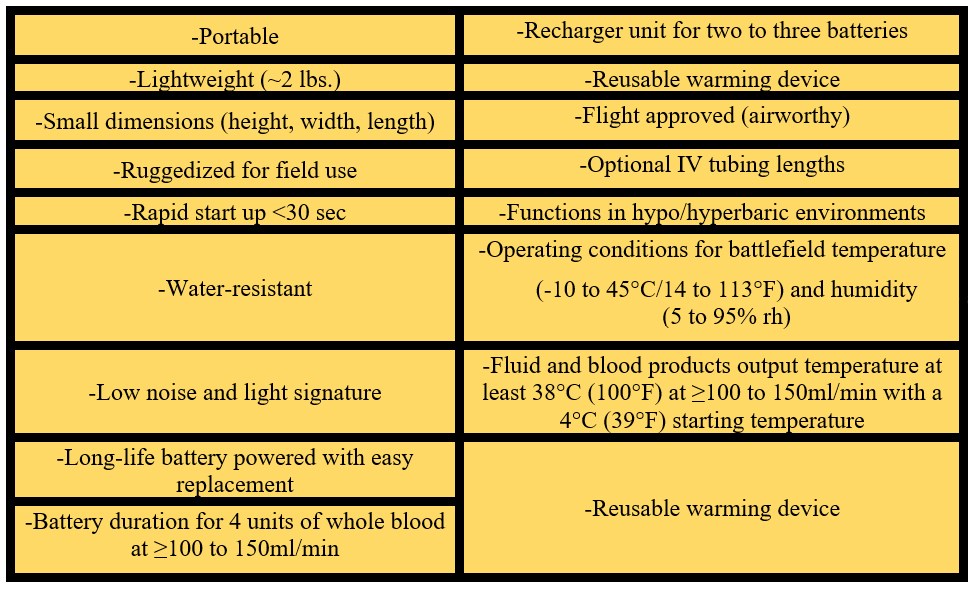
An additional part of a comprehensive hypothermia management strategy for casualty rewarming is an effective, rapid and easy-to-use IV fluids or blood warming device. Previous studies have reported that the performance of these fluid warmer devices varied with flow and initial input temperatures, and many did not deliver fluid temperature between 38-42°C/100-108°F, as recommended. Thus, the CoTCCC Hypothermia Working Group also reviewed and made recommendations for ideal portable IV warmer device characteristics for battlefield application – See Table 4.
Table 4. Ideal Characteristics of a Fluid and Blood Warming Device.
IMPLICATIONS FOR WILDERNESS MEDICINE
In a review of prehospital education sources, an overview of TIH is missing in the majority of wilderness medicine courses, emergency medical service technician courses, and other prehospital care curricula. The focus in wilderness medicine education courses for decades has been about methods to improvise hypothermia wraps for the management of accidental hypothermia victims. Although this is an important skill to learn, this approach is mostly taught as a passive (no active heating sources) hypothermia wrap to prevent further victim heat loss. While a passive hypothermia wrap is certainly the minimum that should be done, it will be insufficient, and not ideal for moderate to severe hypothermia in traumatized victims for they need active heating inside a hypothermia wrap.
The HPMK can be easily transitioned into the civilian programs, such as, EMS, civilian medics on tactical teams, U.S. park medics and rangers, search & rescue personnel, wilderness expedition medical teams, and remote adventure race medical teams. When in cold environments, the HPMK should be augmented into an insulated system by placing the patient inside a hooded sleeping bag as one option. Alternatively, place down-filled clothing around the patient’s torso, neck and head, or wrap the patient in two wool blankets – See Figure 2.
Figure 2. Preferred method to create an insulated HPMK for hypothermia heated wrap. (a cross-sectional view; outer layer to inner layer over casualty). Graphics by G. G. Giesbrecht.
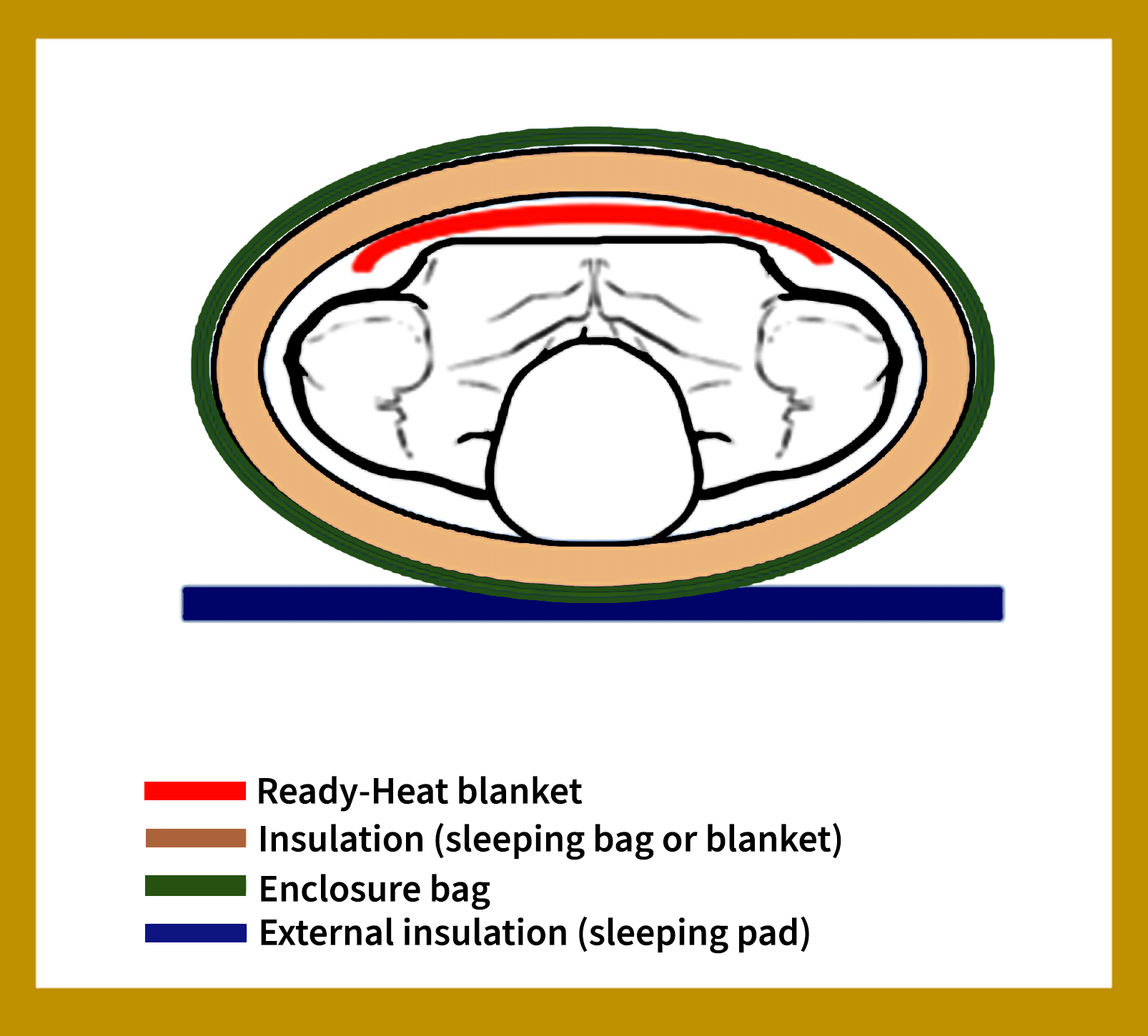
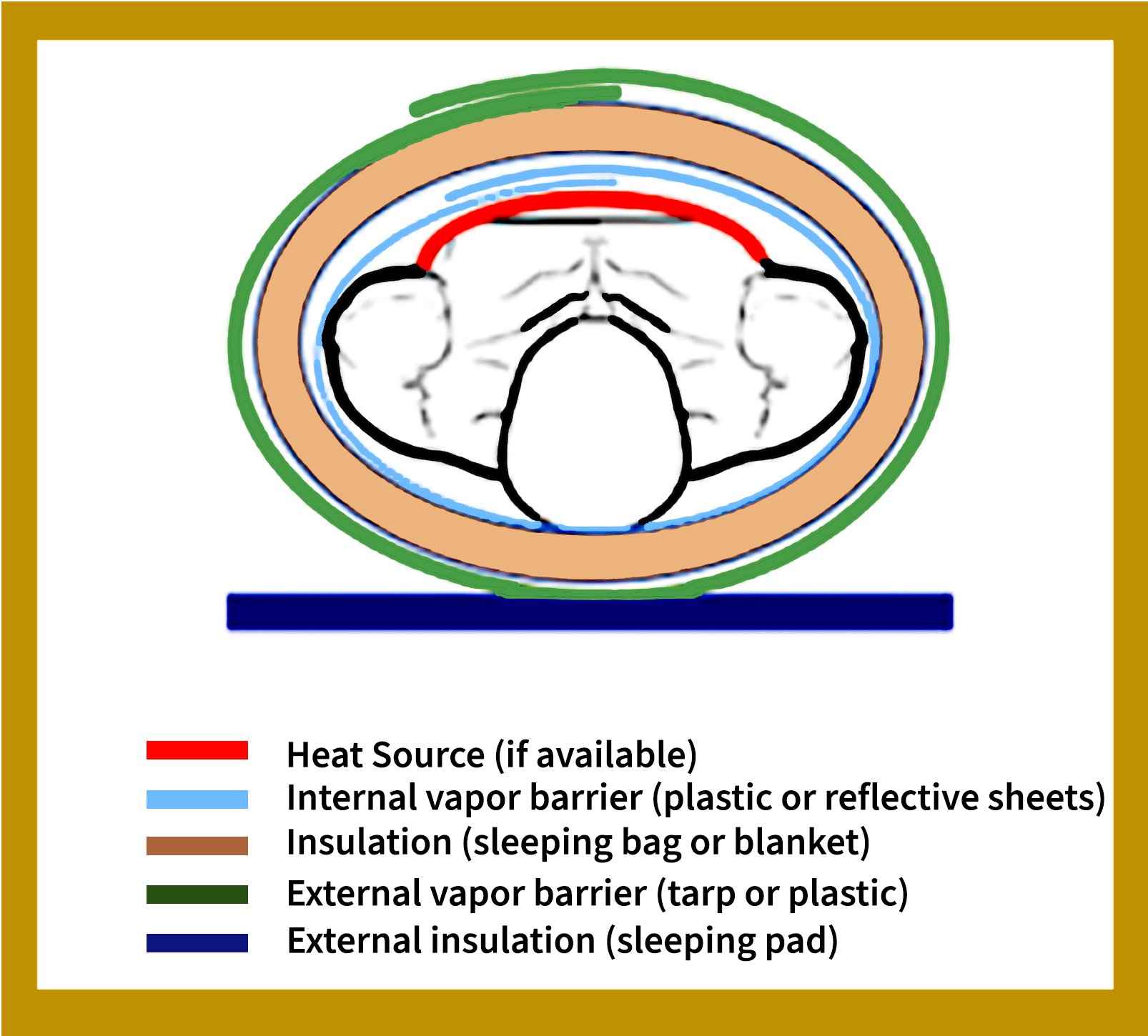
When no HPMK is available, there is good evidence for how to best create an effective improvised hypothermia enclosure system (user-assembled system) as evaluated by Dutta et al. See Figure 3 for cross-sectional layers of an improvised insulated hypothermia wrap.
Figure 3. An improvised insulated hypothermia heated wrap (a cross-sectional view outer layer to inner layer). Graphics by G. G. Giesbrecht.
FINAL THOUGHTS
Mortality occurs more often in TIH victims with much smaller decreases in core temperature when compared to victims of accidental hypothermia. Consequently, prompt treatment with active rewarming is now recommended by the CoTCCC, Prehospital Trauma Life Support, and Advanced Trauma Life Support trauma management guidelines. Furthermore, the Wilderness Medical Society, and International Commission for Mountain Emergency Medicine recommend active heating during hypothermia management. The use of a hypothermia enclosure system, like an insulated HPMK, or an improvised hypothermia wrap with insulation, are essential tools for your wilderness medicine skill set. Furthermore, we recommend an educational initiative to address the gap in all prehospital care curricula that should begin providing course content for both trauma-induced hypothermia and accidental hypothermia.