Introduction
Prior to 2001, tourniquets (TQ) were inferiorly made, lacked evidence and effective training, and their use was discouraged. However, with effective modern TQ science, development, and TQ inclusion into the Tactical Combat Casualty Care (TCCC) guidelines, TQs became universally accepted by 2006 in the military as the primary option for extremity arterial bleeding. Eventually TQ use transitioned with success to civilian Emergency Medical Service/Fire Department personnel, Law Enforcement personnel, and first responders. Yet, there still is a need to overcome TQ myths (Table 1). Additionally, history reveals from WWII to present that mistakes will occur when applying a TQ (Table 2). For instance, many TQs have been applied to injured extremities without life-threatening bleeding in both military and civilian casualties. Many of these applied TQs were inappropriate since many were placed without visualizing the wound when not in a direct threat environment. In addition, when TQs are applied for over 2 hours, there will be progressive damage that may result in muscle necrosis, need for fasciotomy, renal failure, amputation, and death. This suggests a greater need for TQ education and training.
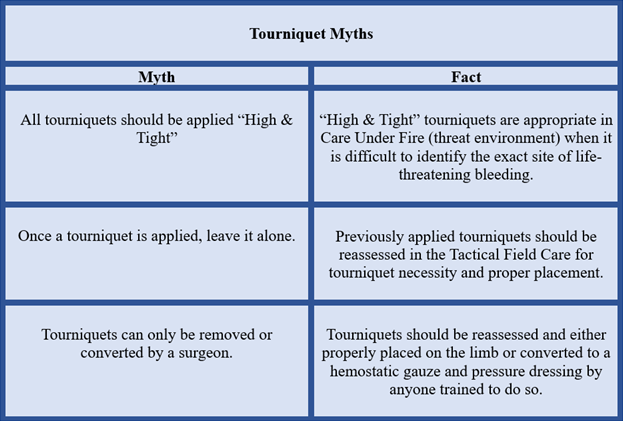
Table 1. Tourniquet myths in TCCC and in any civilian setting. Holcomb et al 2023.
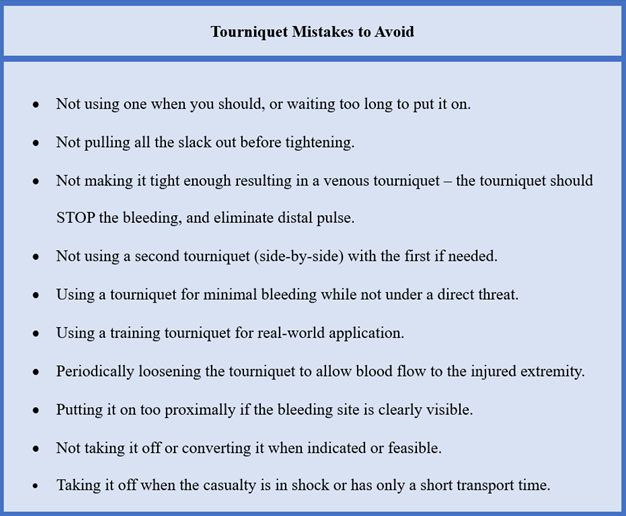
Table 2. Failure points for tourniquet application and removal based on CoTCCC lessons learned.
As an outcome from recent TQ lessons learned in the Ukraine and Israel wars, an article by Colonel John Holcomb, MD and colleagues was recently published in the Journal of Trauma, December 2023. They describe a renewed attention and education about how to avoid prolonged TQ application as recommended in the TCCC guidelines (See Massive Hemorrhage and Circulation sections – Table 3). It is our intent to provide the wilderness medical provider information about: 1) TQ replacement and TQ conversion (ideally performed no later than 2 hours after being applied); and 2) ensure the reader has up-to-date CoTCCC resources with the current TQ replacement/TQ conversion education and training.
Background
The CoTCCC has provided TQ guideline recommendations for application procedures and a timeline when to convert to hemostatic gauzes and pressure dressing - See Table 3. However, the recommendations for TQ conversion were not explicitly detailed until two articles were published in 2015 by Captain Brendon Drew DO, USN, and Colonel Stacy Shackelford MD, USAF. TQ conversion is attempting to convert a TQ to a hemostatic gauze and a pressure bandage. TQ replacement is attempting to exchange a TQ placed “High & Tight” over garments on the extremity with a new TQ placed on the skin 2–3 inches above the life-threatening bleeding site. TQ replacement is also done when conversion to a hemostatic gauze and a pressure dressing is unsuccessful for hemorrhage control, or when the injury caused a total or near total amputation and conversion is not indicated. Both maneuvers focus on minimizing ischemia in healthy tissue. Holcomb et al 2023 have recommended increased education on the indications for TQ replacement/TQ conversion (Table 4).
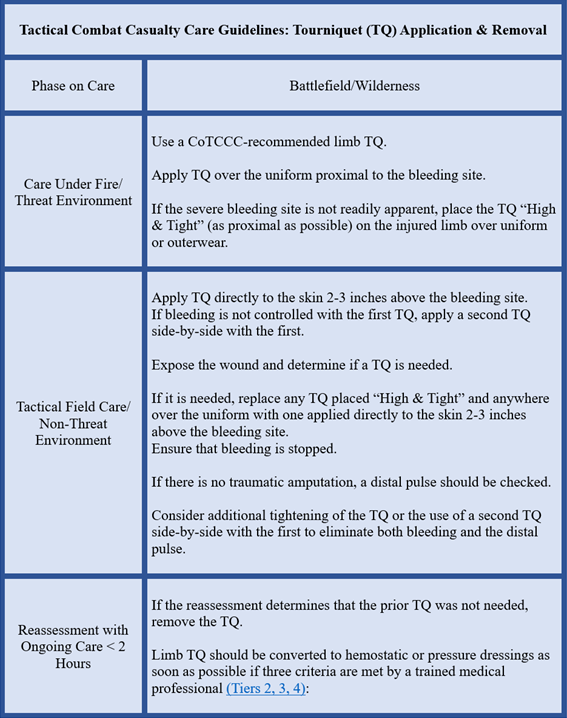
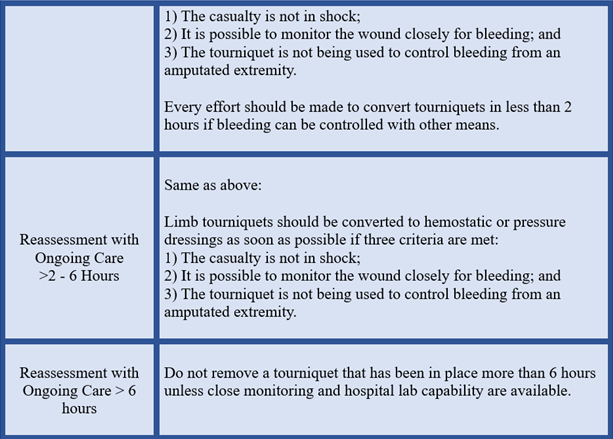
Table 3. Condensed version of TCCC Guidelines (2021) for tourniquet application, replacement and conversion.
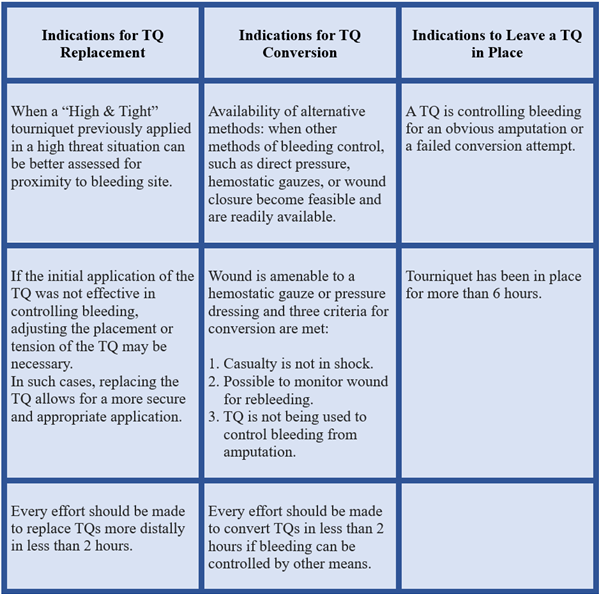
Table 4. Indications for tourniquet (TQ) replacement and conversion recommendations. Holcomb et al 2023
The Problem
Given rapid evacuation transport times over the past 20 years of military conflicts, TQ replacement and TQ conversion were rarely indicated. As a result, providers acquired very little experience with TQ replacement/TQ conversion. More recently, in remote areas of Africa and Indo-Pacific region, operations have shown that prolonged evacuation time will be expected. Unfortunately, this is the same scenario in the ongoing wars in Ukraine and Israel that has resulted in prolonged TQ application without any attempt for TQ replacement/TQ conversion. Several factors, including “High & Tight” TQs being placed outside the direct threat phase, and a lack of medical personnel, contributed to significant morbidity and mortality in the Ukraine. Similarly, in Israel, community members acted as first responders in applying TQs to wounded neighbors during the Hamas assault on their communal kibbutz, but these first responders were without the training for TQ replacement/TQ conversion. In the US, the TCCC guidelines were only updated in September 2023 specifying which personnel (Tier 2, 3, 4) with TQ replacement/TQ conversion training can perform these skills to prevent prolonged TQ time.
Recommended Solutions
Holcomb et al provided a series of recommendations for prolonged TQ challenges in support of the senior surgeons and other clinicians in the Ukraine and Israel, and for US military and civilian personnel. They stated:
- Carry at least two CoTCCC recommended TQs to avoid counterfeit or others that are not evidenced-based without research showing effectiveness and safety that meets the TQ criteria;
- All military and civilian training (medical and non-medical personnel) courses must train and drill the indications for TQ replacement/TQ conversion including the principles of ongoing reassessment of the injured limb with equal importance;
- Should medical personnel NOT be immediately available in the prehospital setting, OR if the TQ has been in place for 2 hours, TQ replacement/TQ conversion should be attempted by anyone who has been trained to perform these tasks.
Training & Education Resources
Based on these lessons learned from the Ukraine, leadership within the Joint Trauma System (JTS) and CoTCCC have developed best practices training resources for TQ replacement/TQ conversion as located in the CoTCCC website deployedmedicine.com:
TCCC Study Guide - A consolidation of the TCCC tourniquet guidelines and procedures.
Tourniquet Application
Tourniquet Reassessment
Tourniquet Replacement
Tourniquet Conversion
TCCC Tourniquet Conversion Training Video
TCCC Tourniquet Replacement Training Video
Application to the Wilderness Medical Provider
Holcomb et al clearly stated that the principles of TQ replacement/TQ conversion are very applicable to the austere and wilderness environments since the medical response to an injured person and the ultimate evacuation to a trauma center will be beyond 2 hours. Consequently, we recommend that anyone (even non-medical) who carries a TQ into the backcountry that you be well prepared to complete TQ replacement/TQ conversion. Previously, we recommended what items to carry as part of your hemorrhage control kit into the backcountry. Also, we recommended to seek out hands-on training on how to correctly develop an improvised TQ, particularly if you decide not to use CoTCCC recommended TQs. The majority of studies comparing commercial versus improvised TQs report that CoTCCC recommended TQs are far superior for rapid access, ease of use, and the ability to stop severe extremity bleeding.
Finally, see the recent article by Kragh et al, that presents evidence for the increased risk of extremity frostbite following the application of a limb TQ. Consequently, it will be essential to provide extra layers of insulation to the affected extremity to prevent tissue freezing, but yet keep the extremity cool and without providing a warming source directly on the ischemic tissue. This rationale is based on hand surgery studies that report a cooler extremity can tolerate longer ischemic duration. There is also a single case report of a military aviator who landed his helicopter on a snow-covered mountain top during a tactical mission, and was shot in the hand/wrist. He survived without an amputation or loss of extremity function following 16-hour TQ application.
Final Thoughts
Battlefield tourniquets are estimated to have saved up to 2,000 US soldiers’ lives in the past two decades in Afghanistan and Iraq. However, it is essential to recognize the common TQ mistakes, such as prolonged use over 2 hours without TQ replacement/TQ conversion. Initially, TQ replacement and TQ conversion were conducted only by trained medical personnel. However, a key takeaway point from Holcomb et al 2023 is that TQ education and skills training are essential for all military service members and civilians, and for anyone in austere/wilderness environments, so that they are trained to safely apply, convert, or replace a tourniquet.