Hantavirus cases are on the rise in the state of Arizona. Since 2012, no more than five cases per year have been observed in this state. However, in this year alone, authorities have already accounted for nine cases, with three deaths.
Hantavirus is found throughout the Southwest, with 94% of the cases occurring west of the Mississippi River. Hantavirus is primarily transmitted by deer mice. The virus can be found in fresh urine, droppings, and nesting materials. Why hantavirus cases have surged only in Arizona state remains unclear. Experts suggest that the increase in rodent population density, combined with climate change and more intense heat waves, may be driving rodents closer to human populations in Arizona. Rainy weather and flooding increases the chance of the rodents coming closer to people because they often end up seeking shelter in barns or human dwellings.
Underreporting of cases is also a possibility, as the symptoms of hantavirus can resemble those of many other viral illnesses, potentially delaying an accurate diagnosis until the illness has progressed. According to the CDC, households with children under 5 years old, pregnant women, or individuals with weakened immune systems are advised against keeping pet rodents, including rats, as they are at higher risk of severe illness.
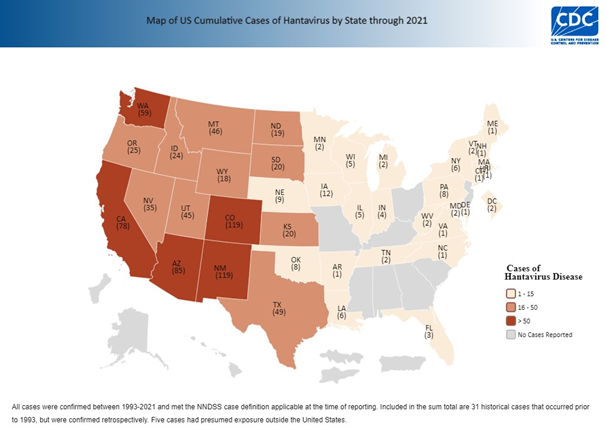
Map of cumulative cases of Hantavirus by State through 2021. Source: CDC
An acute Hantavirus infection is characterized by non-specific viral symptoms such as muscle pain, fatigue, and fever, and in the serious cases can cause respiratory distress and severe pneumonia. Hantavirus Pulmonary Syndrome is a severe and potentially deadly disease that affects the lungs. Symptoms usually start to show 1-8 weeks after contact with an infected rodent. Four to ten days after the initial phase of illness, the late symptoms of HPS appear, which include coughing, dyspnea, and respiratory failure requiring mechanical ventilation.
The mortality rate of hantavirus pulmonary syndrome (HPS) is high, with nearly 38% of affected patients not surviving. The primary risk factor is exposure to rodents, particularly in homes situated in rodent-infested areas. In addition to household exposure, certain occupations—such as herding, farming, construction, and cleaning services—also carry a higher risk of hantavirus infection. Recreational activities in outdoor environments where rodents are present further increase the likelihood of exposure.
The treatment for hantavirus infection is mainly supportive, including rest, hydration, and symptom management. Patients with a history of rodent exposure should be reported to the local health department or the CDC's Emergency Operations Center at 770-488-7100.
To avoid hantavirus, it is best to avoid close contact with rodents and their droppings. Some rodent contact may not be controlled, such as exposure to contaminated freshwater after heavy rains or floods, or through consumables that are stored in garages, barns, or warehouses. Special attention should be given when cleaning a space where there was recent rodent activity. You may accidentally breathe in hantavirus-contaminated air when cleaning up after rodents, or touching contaminated objects and then touching your eyes, nose, or mouth.
These viruses possess a double lipid-layer envelope, which makes them vulnerable to various disinfectants, including industrial Lysol, sodium hypochlorite solution, 10% Lysol, and 70% ethanol. When cleaning potentially contaminated environments, it is recommended to use one of these disinfectants on a damp cloth to avoid creating aerosols. The cleaning process should be carried out while wearing N95 masks, and it's advisable to ventilate the area before and after the process.
If you are camping in an area where Hantavirus is endemic, avoid leaving food exposed, as this attracts animals. Remember that most rodents are most active at night, and they may be around even if not noticed. You may also be exposed to the virus after swimming, rafting, or paddling in endemic areas. Water should be boiled, treated with chlorine, or exposed to UV to kill hantavirus.