We all know the WMS has great education. What happens after you’ve been a member of the WMS for several years, have become a fellow of the WMS (FAWM), and perhaps have also completed your Diploma in Mountain Medicine (DiMM)? You’ve gained all this expertise and have a passionate love for the outdoors. What’s the next step? How can you apply what you’ve learned? Many of us are struggling with this question. How do we share our knowledge and use our skills?
How about becoming a medical director or medical advisor? The expertise can be helpful to a myriad of organizations, from a local small outdoor guiding company, to a local fire department, to that youth soccer organization where you’d like to be available for games on the side should injuries occur. Organizations such as National Outdoor Leadership School (NOLS) and Outward Bound frequently are asked whom they might contact to provide medical direction. Some organizations don’t even know how they would benefit from your knowledge. Imagine being the first medical director for your local backcountry outfitter – you can provide education and help improve the quality of care delivered in those rare emergencies, all the while helping your local community. Only sometimes are fees provided to medical directors; however, this is generally not a reliable source of a solid income stream. Most of us provide these services because it’s fun to contribute back to our communities, and it provides an opportunity for us to share our medical knowledge of the wilderness.
There are many members of the WMS who already are medical directors, from very small organizations, all the way to statewide and national parks systems and search and rescue programs. But if you are new to this arena, becoming a medical director may seem like a leap.
A number of WMS members have been discussing the challenge of medical director and medical advisor roles for several years, and would like to create a program within the WMS that supports its members in making this transition. In short, the purpose of this article is to attract interested WMS members to help us!
In order to become a medical director, there are important questions to consider:
1) Liability Insurance: How will you protect yourself? Do you have your own malpractice insurance that will cover activities outside your typical practice environment? Most medical malpractice does NOT cover you outside your typical practice environment – e.g., an emergency physician provides services in a defined emergency department; an anesthesiologist provides service in a defined network of operating rooms. While medical lawsuits are rare in wilderness medicine, they can occur and you wouldn’t want to put yourself at risk. Also, for those providing medical direction in a Wilderness EMS perspective, the direction you offer could involve termination of credentials, which can result in job loss for providers working under your oversight. Medical malpractice does not cover you for this liability but employment-related coverage does.
Some organizations will clearly provide, in writing, insurance for the medical director; but if you haven’t asked and seen it in writing, are you comfortable with your risk? Some organizations will also provide compensation, in cash or in kind, to offset your services or insurance. The Good Samaritan Law is an option, but varies from state to state and requires that no compensation be given – but what defines compensation? Did they give you a free drink for helping with a medical event on an airplane? Do you get a pro deal on gear for your services? Some lawyers would successfully argue you’ve been compensated.
Another challenge to utilizing Good Samaritan legislation is that you cannot have a pre-existing duty to treat (or direct others in treatment). If you have a contract with an organization to be their medical director or medical advisor, it could be argued you do have that pre-existing duty to their clients. If you want to obtain your own policy, this can easily run $4,000 - $5,000 per year. Is there an option to find a group policy for multiple people with the same credentials in order to decrease these costs? Again, we are seeking help!
2) Protocols: There are some outstanding general protocols available. NOLS will sell you their protocols for $149. You can create your own (free but labor intense). Perhaps the WMS should coordinate an internal database of protocols? What are the criteria for access to these? FAWM, MFAWM, or DiMM grads? Good protocols are concise, easy to understand, and as much as possible backed by good research, with references. Protocols range from simple wound care, to spine injuries, to CPR, to giving epinephrine. As a medical director, will you equip your teams with medications, and if so, what types? Some like epinephrine are increasingly accessible even to laypeople; others like opioids remain highly controlled and carry significant medicolegal risk for those prescribing them. These are all important questions to answer.
3) 24/7 Coverage: If someone within your organization has a question and needs on-line medical direction, who is available to answer it? As the medical director or advisor, are you offering your availability 24/7? What if you are unavailable? The University of Utah is currently working to create a service that provides 24/7 coverage through their Emergency Department. Is it possible to contract with their service? Perhaps it would be worth exploring a concept similar to the Divers Alert Network (DAN) which offers a 24-hour FREE emergency hotline. Should the WMS work towards providing this invaluable service? If so, again, how is malpractice covered?

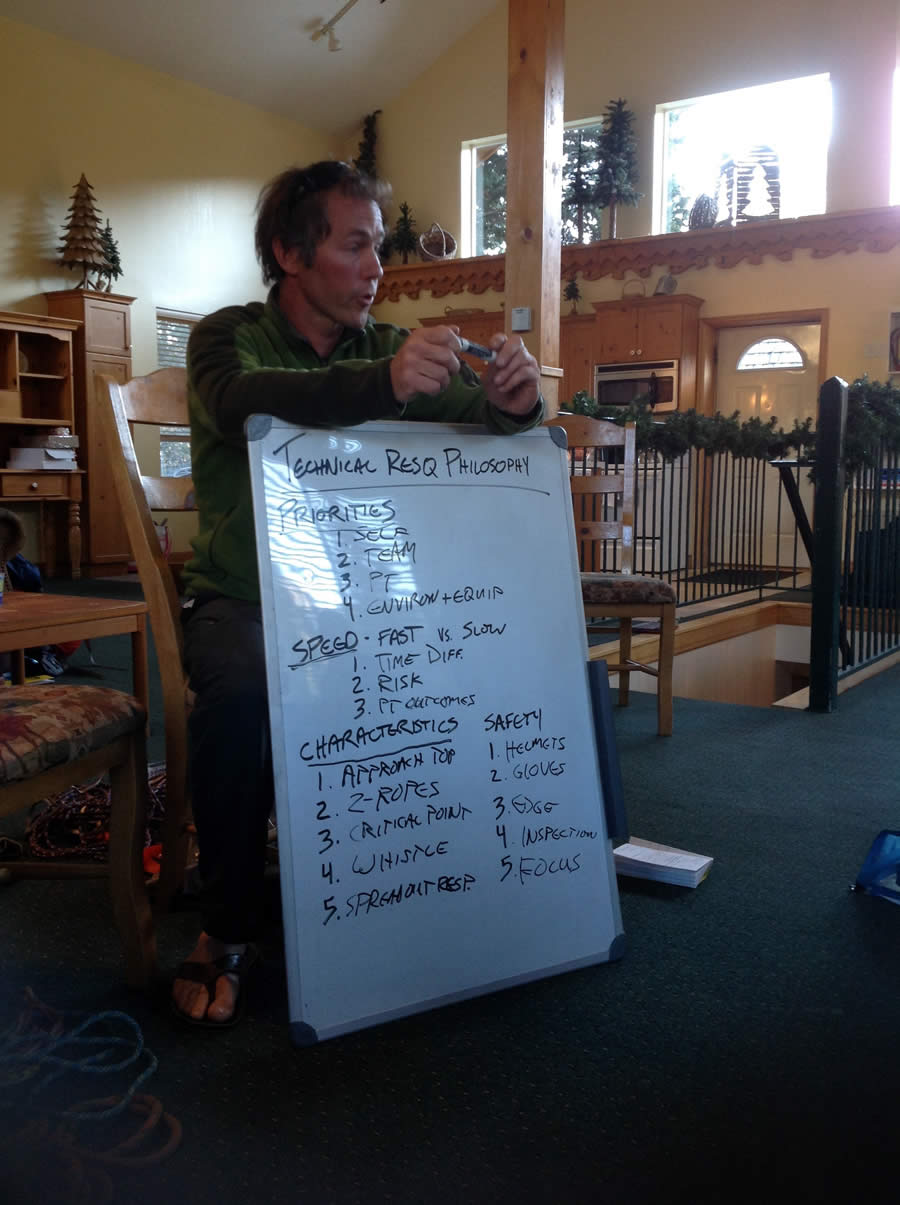
The WMS has members with valuable experience to share with these important concepts. In Jackson Hole in 2014, the Wilderness EMS Medical Director Course was offered as a pre-conference, and will be offered again at the 2016 Park City conference. But the above questions remain.
If you are interested in helping the WMS figure out if it can provide these services, we invite you to join the conversation! You needn’t be a physician, as we all can provide assistance in answering the above questions, and we all have valuable input. The need exists and we strongly believe this can provide another answer to the question of “What does the WMS do for me? Or what can I do for the WMS?”
Depending on the amount of interest we can schedule a phone meeting, video chat, or even small breakout session in Park City at the Mountain Medicine Conference in February.
Hope to hear from you soon!!
Sincerely,
Jamie Lieberman, MD, FAWM, DiMM
Emily Sagalyn, MD, MPH, FAWM, DiMM
Jay Lemery, MD, FAWM
Photos courtesy of James Lieberman
Posted on November 13, 2015