The latest news about peanut allergy is that exposing babies to peanuts early in life may mitigate future risk. This is good news for the new generation of happy campers who one day may be able to relax and enjoy a PB&J after that long hike up the mountain. But for now, the risk of anaphylaxis, a severe, potentially life-threatening allergic reaction, remains for many people allergic to peanuts, other nuts, and other foods. For those who work and play in an outdoor setting, anaphylaxis is most commonly caused by insect stings (bees, wasps, and fire ants are the most dangerous), and in some cases, exercise and exposure to cold temperatures. Other risk factors are latex and medications; asthma is a risk for fatal anaphylaxis.

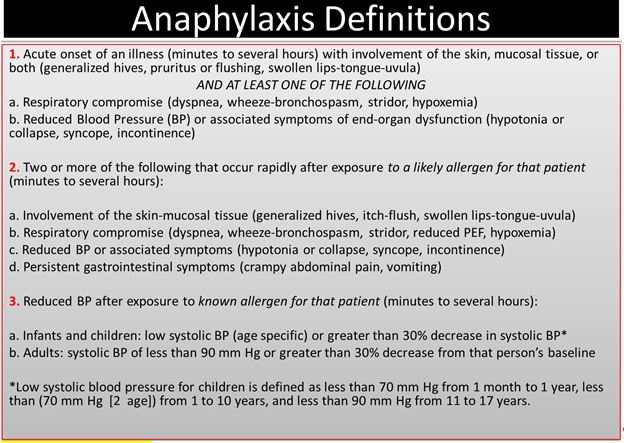
In the US, the overall risk of anaphylaxis is estimated at 0.05 to 2 percent, with 150 deaths/year (this number is higher when reactions to medications are considered). But the prevalence and incidence of anaphylaxis is difficult to estimate due to the current lack of recognition and lack of accepted criteria for diagnosis, although consensus on these is being developed. A 2006 National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network consensus definition (Table 1) has been published in both the emergency medicine and allergist literature, which substantially expand and clarify the definition of anaphylaxis. The standard of treatment is early recognition and administration of epinephrine. Other medications that may be administered adjunctively include antihistamines (both standard antihistamines like diphenhydramine [Benadryl] and H-2 blockers like famotidine [Pepcid]), IV fluids, and corticosteroids.
Route of Administration and Dose of Epinephrine
The preferred route of administration of epinephrine for anaphylaxis is intramuscular (IM) into the anterolateral mid-thigh. In the wilderness setting, epinephrine auto-injectors (EAIs) are most often used. EAIs can penetrate clothing. Popular brands in the US are Epi-Penâ and Auvi-Q.ä The cost is high: approximately $350-500 for a 2-pack, with a fairly short expiration date. Epinephrine may also be drawn manually from a vial or ampule into a syringe and administered IM with the appropriate needle (the dose is 0.3 to 0.5ml of the 1:1000 concentration). This method is less expensive than the EAI as the vial is cheaper and multiple doses can be withdrawn, but more errors can potentially occur. The IM route has been found to be superior to the subcutaneous (SQ) route. Injection site is preferably in the thigh due to more rapid onset of action, but the deltoid may also be used.
.jpg)
It is important to note that a second dose of epinephrine may be needed inpatients who have "biphasic" anaphylaxis. This should be administered 5-15 minutes after the first dose. All patients who have experienced anaphylaxis in the field should receive definitive care after receiving epinephrine. The true incidence of biphasic anaphylaxis is controversial. Previous studies have shown incidence rates of 0.5 to 20 percent. A 2014 study, the largest to date analyzing biphasic reactions, showed an incidence of less than 1 percent.
Settings for Administration of Epinephrine Outside of a Healthcare Setting
Three possible settings for recognition of an anaphylactic reaction and administration of epinephrine outside of a healthcare facility include schools, interaction with the EMS system, and outdoor education and wilderness settings.
Schools
The CDC has issued voluntary guidelines for managing anaphylaxis in schools, including training non-healthcare professionals to recognize the signs and symptoms and administer epinephrine when appropriate. The American Red Cross Council on First Aid and Safety, AMA, and AAAI all support epinephrine administration by the lay public. The majority of states in the U.S. have passed laws requiring schools to create emergency preparedness plans to manage anaphylaxis that include stocking epinephrine. See the following links for further information.
Centers for Disease Control and Prevention. Voluntary Guidelines for Managing Food Allergies in Schools and Early Care and Education Programs. Washington, DC: US Department of Health and Human Services; 2013.
School Access to Emergency Epinephrine Law
EMS
In a position statement, the National Association of EMS Physicians (NAEMSP) recommended that emergency medical responders (EMRs; first responders) be allowed to carry and administer EAIs to patients with anaphylaxis, with the caveat that there be 1) physician oversight, 2) additional training for EMRs in the recognition and management of anaphylaxis, and 3) quality assurance programs.
Currently, all 50 states allow administration of epinephrine by paramedics, and a number of states require that EMTs also carry the drug.
National Association of EMS Physicians. The Use of Epinephrine for Out-of-Hospital Treatment of Anaphylaxis. Prehospital Emergency Care 2011 Oct-Dec ;15(4) :544-[CHECK THIS]
Jacobsen RC, Millin MG. The Use of Epinephrine for Out-of-Hospital Treatment of Anaphylaxis: Resource Document for the National Association of EMS Physicians Position Statement. Prehospital Emergency Care 2011;15:570-576.
WMS and Outdoor Education, Wilderness Settings
The administration of epinephrine in an outdoor education or wilderness setting is murkier. Some outdoor education programs and organizations have been training their first responders to administer epinephrine for decades. Now the legality of this is being questioned:
- Can a physician write a prescription for an outdoor organization rather than a specific individual? In the US, a physician must write a prescription as the drug cannot be purchased without one; other countries may have different laws.
- Pharmacists can't dispense a prescription to an organization (so should every participant carry their own prescription?).
- Is it legal for a physician to write a prescription for an individual (they have not seen) to use on a third party?
- Can a nonmedical professional with first aid training legally administer epinephrine (which has to be injected) in a medical emergency? Is this the illegal practice of medicine without a license, even if the intent was to help? Is the rescuer protected by Good Samaritan laws?
- Can an organization that allows their staff to administer epinephrine lose their liability insurance as it does not cover an illegal act (answer: potentially yes)?
As discussed above, many states have laws stating that nonmedical personnel such as teachers can administer epinephrine in a school setting, but this may not extend to activities outside the school, including wilderness settings. However, there are exceptions. For example, in North Carolina physicians can legally train people to administer epinephrine in the field, New York requires camp counselors to be trained to administer epinephrine, and Alaska has the most comprehensive law that includes coverage for writing a prescription (training required) and most importantly, immunity from liability. There are also other states that allow epinephrine administration by nonmedical or lay people working in outdoor settings after proper training and/or certification. The most important take away is that you must know the laws in your state.
[Reference: Brown RE. "Outdoor Law: The Legal Structure of Teaching and Administration of Epinephrine in Wilderness Emergency Situations." 2006.]
WMS Practice Guidelines for Epinephrine Use
In the 2014 update to the 2010 practice guidelines, WMS supported the concept that "properly trained, nonmedical professionals whose work responsibilities require them to provide emergency medical care be trained to appropriately administer epinephrine for the treatment of anaphylaxis."
[Gaudio FG, Lemery J, Johnson DE. Wilderness Medical Society Practice Guidelines for the Use of Epinephrine in Outdoor Education and Wilderness Settings: 2014 Update. Wilderness & Environmental Medicine 2014;25:S15-S18.]
WMS is working to change this concept into actual law.
WMS Practice Guideline (PG) for Outdoor Education and Wilderness Setting Programs Operating Procedures and Staff Training Curriculum for Administration of Epinephrine:
- All staff authorized to treat anaphylaxis must be trained by qualified instructors or programs (see WMS PG for specifics)
- Staff authorized by institution to administer the patient's own medication or that provided by organization
- Development of organizational field protocol
- Establishment of quality-assurance program (see WMS PG for specifics)
- Oversight by a medical consultant/advisor or a medical control
Examples of field protocols for administration of epinephrine for anaphylaxis have been developed by wilderness medicine training programs such as Wilderness Medical Associates, NOLS, and Wilderness Medicine Outfitters. These can be found in the "supplementary materials" of the 2014 WMS Practice Guidelines.
Posted on April 8, 2015