Ask the physicians at Kathmandu Model Hospital (KMH) if they practice wilderness medicine, and they will look puzzled by the terminology. But in fact they practice it daily. A patchwork of wireless connections beams from chaotic Kathmandu, bounces off remote Himalayan peaks and transmits information to KMH. Specialists in Kathmandu advise providers in remote outposts using the time-tested skills of assessment, stabilization, treatment and triage: the backbone of our own wilderness medicine practices.
Wilderness medicine and telemedicine share a common function of providing healthcare in austere and remote areas, albeit via different methods. Wilderness medicine is considered a hands-on field discipline that uses scant equipment and supplies. Telemedicine utilizes off-site providers to deliver patient care via telecommunications. The two disciplines have a natural symbiosis. One provides practicality and emergency skills and the other provides the means to deliver.
Remote communications in medicine have been around for centuries. Smoke signals were sent from Native American villages to warn of contagious diseases. In the early 1900s Australians communicated via two-way radios to the Royal Flying Doctor Service. About 40 years ago telemedicine hit the USA for cardiac resuscitation and has expanded globally ever since. Now there’s even a professional society, American Telemedicine Association.
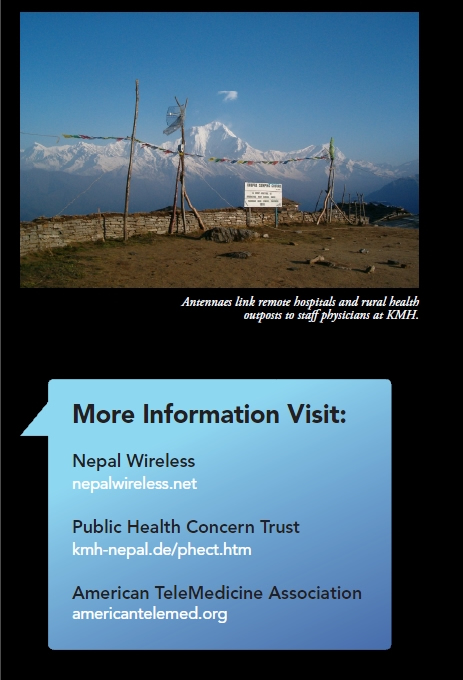
In Nepal these disciplines have been blended by a unique partnership between Nepal Wireless, the brainchild of entrepreneur and educator Mahabir Pun and Public Health Concern Trust known as Phect-Nepal, a private NGO. In 2007 Mr. Pun set up a project at Kathmandu Model
Hospital, to reach more remote hospitals and rural health outposts
Whereas remote hospitals are staffed by physicians, nurse anesthetists and nurses, the health outposts are staffed nurse midwives or healthcare workers (HCW) who have one to two years of training. Akin to wilderness medicine, they provide healthcare with limited supplies, few medications, and outdated or malfunctioning equipment. What’s more, they lack access to continuing medical education. In 2003, armed with a $10,000 grant, four UCLA students installed the wireless network using old, new and repurposed equipment. The connection was laboriously connected from Nangi Village in Myagdi District to Pokhara, the largest city in western Nepal. This connection was expanded to Kathmandu in 2006 and now includes Internet and phone service.

Fifteen off-site hospitals, health centers and sub-health posts can tune in up to six times a week during morning reports at KMH using a desk or laptop computer and video camera connected to the wireless network. KMH provides video conferencing capability with cameras installed in their conference room and connected to a large screen television. The KMH staff physicians and junior medical officers discuss their cases and provide consultations; often advice is based on WMS Wilderness Medicine Practice Guidelines. Connectivity is an expected problem in developing nations. Just as it is difficult to provide healthcare in resource-poor environments, it is challenging to provide wireless access in electricity-poor countries. Nepal suffers from up to 14 hours per day of load shedding, when electricity is cut off and diverted elsewhere, often resulting from lack of water to generate power. A key advantage of telemedicine is reduced cost. Villagers avoid lengthy and costly trips to an advanced level of care facility, which are sometime several days walk. It has reduced the cost of travel to obtain continuing medical education for the HCW by providing wilderness education on-site. It has improved remote practitioners clinical practice by increasing their knowledge, skills, self-esteem and reducing their isolation. This translates in any language to better patient outcomes. Many healthcare systems in developing areas of the world use similar telemedicine systems to provide care but may not recognize the value of wilderness medicine skills and education as a means to manage the care. The union of Nepal Wireless and KMH stands as a resource and example for future projects.