On July 26th, 2008, I toed the starting line of a 7-mile race in Iowa alongside a few thousand other runners. It was 28.9°C (84°F) with 93 percent humidity that day. The throngs of people moved slowly. Weaving in and out of the crowd, I trudged on for the first five miles. Then the crowd opened up and I was able to really let loose over the last two miles. I crossed the finish line and slowed to a walk an hour after beginning the race. As I did, I was suddenly overcome by feelings of sudden flashes of heat, followed by icy cold. My vision began to blur and my legs cramped; I was beginning to experience exertional heat illness.
Heat and the body
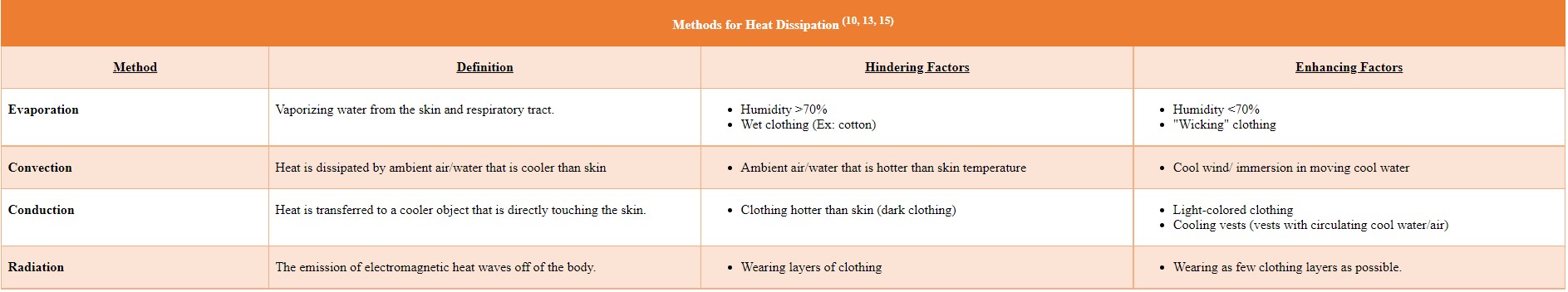
The body builds up heat through physical activity as well as from radiation from the sun. It corrects this by dissipation of that heat through different methods. If these methods are overwhelmed, the basic lipids and phospholipids of the body’s cells begin to destabilize. This in turn leads to cardiovascular collapse and eventually multi-organ failure. The exact temperature of this failure is different for every person, as it is dependent on many factors, but as a general rule, if a person’s temperature is greater than 41°C (106°F) the person should be emergently treated.
Adaptation to Heat
The human body not only has the ability to dissipate great amounts of heat, it also has the ability to further acclimate itself to increased temperature. The body acclimates itself to heat in several ways: plasma volume expansion, increasing blood flow to the skin, increasing sweat output, decreasing threshold for initiating sweating, lowering the salt concentration of sweat, and decreasing the core and skin temperatures for a standard exercise.
Impediments to heat loss
Physical features that impede heat loss include poor physical fitness, low skin-area-to-mass ratio (e.g., obesity, large muscle mass), and lack of heat acclimatization.3 Dehydration will increase the heat your body makes by 0. 22°C (0.4°F)/one percent total body weight loss.15 Certain medications can increase risk of EHI including: antihistamines, decongestants, tricyclic antidepressants, amphetamines, beta-blockers, and diuretics. Large areas of scarring decreases the amount of viable sweat glands. Lastly, there are several conditions that can contribute to EHI, including old age, peripheral arterial disease, heart disease, and diabetes mellitus. (5, 15, 18)
EHI Defined
- Heat Cramps: Technically a misnomer, as hyperthermia is not a requisite. Characterized by intense muscle pain, prolonged persistent contractions of muscles, and spasm. Thought to be due to a combination of electrolyte imbalance, dehydration, and neurogenic fatigue.
- Heat Induced Syncope: Loss of consciousness that happens shortly after exercise. Thought to be due to an abrupt decrease in venous return once an athlete completes the event.
- Heat Exhaustion: Criteria to meet this include: inability or difficulty in continuing to exercise, core body temperature of 101 – 104°F at the time of collapse, and no significant Central Nervous System (CNS) dysfunction (seizure, altered level of consciousness, delirium).
- Heat Injury: Defined as EHI with both hyperthermia (104-105°F) and end organ damage, but without significant neurological manifestations. Commonly injured organs are: muscles, kidneys, and liver.
- Heat Shock: Multisystem injury characterized by CNS dysfunction and a core body temperature greater than 104°F.
Prevention of EHI
The prevention of exertional heat illnesses begins with proper planning and preparation, including location, acclimatization, hydration, and clothing. When thinking of a location, one must consider the heat and humidity he or she will encounter in a given location. Acclimatization to heat/humidity should take place over the course of 10-14 days, with daily incremental increases in exposure to hot environments. Temperature should be greater than 26°C (78.8°F). If that temperature cannot be attained, extra layers of clothing should be added to simulate heat. Aerobic exercise should be maintained at 60-80 percent of maximum heart rate (MHR = 220 – age) for greater-than-or-equal-to 60 min/day. Another option is post exercise, exercise being classified as cardio at 65 percent MHR for 40 min at 18°C (64°F), immersion in 40°C (104°F) water for 40 min/day over six days.19 Staying hydrated is key when participating in activities in the heat; it is important that a person keep from becoming greater than two percent dehydrated (less than two percent loss of your body weight in water loss). Clothing should allow quick cooling or retention of less heat, a wicking material is preferred and materials such as cotton that hold water should be avoided. Dark-colored clothing should also be avoided as they can trap heat. A drawback to light-colored clothing that must be considered is the increased risk of sunburn while wearing it, unless of course it has an SPF rating.
It is also important to reduce the risk of EHI during an exertional activity. The first method is drinking an ice slurry before and during exercise; this reduces core body temperatures by 0.5-0.66°C (0.9-1.2°F), with the temporary side effects of “brain freeze” and abdominal cramping. The second is arm immersion cooling, which lowered core body temperatures by 0.7°C (1.25°F) when a person immerses his or her forearms in 10-20°C (50-68°F) water for 10 minutes during rest work cycles. This is effective because of the high vascularity of the forearm and water being better for heat transfer as compared to air (24 times greater). (9,13) Another method tested was taking four mandatory 15-minute rests during the initial two days of a seven-day, 157.8-mile (254 km.) ultramarathon race. In this study, the institution of mandatory rests decreased the number of “did not finishes” related to exertional heat illnesses from 54.3 percent to 15.4 percent, indicating that these rest stops improved safety amongst the athletes as well as increasing their acclimatization.11
Treatment of EHI
Active treatment of hyperthermia has many options, but the two mainstays of treatment are cold-water immersion and evaporation therapy. Cold-water immersion has the best results (see table below for typical cooling rates).18 If someone has suspected EHI, he or she should be immersed for approximately 15-20 minutes with his or her rectal temperature being monitored if possible. Older persons do not tolerate this as well as younger persons.(5,18) Another option for those who aren’t able to tolerate immersion (or if it isn’t available) would be evaporation using spray and fan. When using evaporation the patient should be kept moist and fanned constantly.14 If immersion or evaporation aren’t available, cover the patient in packets of crushed ice; this has been found superior at cooling patients than cooling with chemical packets or ice solely on the groin, axilla, and neck. Numerous other methods have been studied: cold showers, moving to a shaded area and placing cool/cold wet towels on as much of the body surface as possible, and immersing hands in cold water. These have been found to be less effective than the three methods described above.